Prostate
Prostate cancer is one of the most common cancers in men. On an annual basis, approximately 1.1 million men are diagnosed with prostate cancer across the world. Texas Radiotherapy offers cutting-edge treatment for prostate cancer including brachytherapy, intensity-modulated radiation therapy (IMRT), and stereotactic body radiation therapy (SBRT/SRS). Not only does Texas Radiotherapy offer cutting-edge treatment options, we also perform better and safer prostate biopsies utilizing MRI-guidance and a transperineal approach to better diagnose and stage prostate cancer.
Overview
Prostate cancer is most commonly adenocarcinoma that originates in the cells of the prostate. The prostate gland is a small walnut-sized gland that is part of the male reproductive system. Typically, prostate cancer grows slowly and is often confined to the prostate gland. There are many prostate cancers that can be watched and do not require treatment. However, some cases are much more aggressive and can spread or metastasize quickly. Prostate cancer that’s detected early with screening is highly curable.

STEPS IN UNDERSTANDING AND CONQUERING YOUR CANCER:
1) PSA Test: if you haven’t had your PSA test but think you may have prostate cancer based on symptoms, then you can schedule with Dr. Cavey for a PSA test and diagnosis, or he can refer you for a PSA test. A short consultation will provide you with the best steps your personal and medical situation.
2) Proper Diagnosis: Dr. Cavey uses the newest diagnostic techniques to ensure that your diagnosis is correct. A correct diagnosis also improves your outcome.
Knowing your PSA is critical for your best outcome.
Dr. Cavey provides a treatment plan built just for you.
If you're dealing with a high PSA number, this video will introduce you to some of our prostate cancer patients and survivors.
Course of Treatment
Most of the time, there are no signs or symptoms of prostate cancer. Symptoms arise when Prostate cancer is discovered at an advanced stage. These symptoms can also occur with non-cancerous conditions such as benign prostatic hypertrophy (BPH) or prostatitis.
Symptoms include:
- Difficulty starting the urinary stream
- Weak urinary stream
- Blood in ejaculate
- Pelvic discomfort
- Bone pain
- Erectile dysfunction
Screening should typically begin at age 45 or earlier at age 40 if there is a family history or in African Americans.
- Digital rectal examination (DRE). Your doctor inserts a gloved and lubricated finger into the rectum to feel for any nodules in the prostate and to estimate prostate volume.
- Prostatic specific antigen (PSA). Prostate cells produce an enzyme named Prostate Specific Antigen or PSA. The PSA is measured by a routine blood test that detects a protein produced solely by prostate cells. It is elevated in prostate cancer, but also in some non cancerous conditions (BPH, infection, inflammation). Elevated levels of PSA are often the first sign of prostate cancer. It is used in the diagnosis of prostate cancer, but also during follow up after treatment to determine if the cancer is gone.
If a DRE or PSA test raises concerns, your doctor will likely recommend a biopsy.
Diagnosing prostate cancer Biopsy
Approximately one million men in the United States undergo a prostate biopsy to detect suspected prostate cancer each year. There are two types of prostate biopsies: transrectal ultrasound-guided biopsies (TRUS) and MR-fusion transperineal biopsies.
- Transrectal ultrasound-guided biopsy of the prostate (TRUS).
- TRUS is the most common approach to performing a biopsy which is performed by using an ultrasound probe in the rectum, and then samples are obtained by passing a needle through the rectal wall into the prostate. This biopsy method takes samples from multiple standard sites with no specific lesion target.
- MR-fusion transperineal biopsy of the prostate.
- Texas Radiotherapy utilizes the MR-fusion transperineal biopsy which is an advanced technique for performing biopsies that is being used increasingly to improve the accuracy of diagnosing prostate cancer. Fusing real-time ultrasound images with pre-exam MRI data provides better guidance to help accurately target lesions identified on the MRI, potentially reducing the risk of missing high-grade tumors or understaging tumors during active surveillance.
The MR-fusion transperineal biopsy is an improvement over the traditional transrectal ultrasound method because the MR-fusion transperineal biopsy targets specific lesions versus random sampling. Additionally, transperineal biopsies can reach parts of the prostate that are nearly impossible to reach during a transrectal biopsy. Transperineal biopsies are much “cleaner” than transrectal biopsies and have less risk of infection. Transperineal biopsies can be performed in the office with local anesthesia or in the operating room under general anesthesia. Patients have reported less discomfort with transperineal as opposed to transrectal biopsies. The MR-fusion transperineal technique is now the standard of care for prostate biopsies.
Imaging
In some instances, CT scan, bone scan or PET scan may be requested for staging purposes, i.e. to determine if there are signs of cancer spread. These tests are usually only requested for patients with more aggressive disease (unfavorable intermediate or high-risk).
Staging Gleason’s score
When a biopsy confirms the presence of cancer, the Gleason’s score determines the level of aggressiveness of the cancer cells or the Grade. The score is comprised of the primary cellular pattern + the secondary pattern or appearance of the cells. Each pattern is scored from 1 to 5, with 1 being least aggressive and 5 being most aggressive. Prostate cancers are actually scored from 6 – 10. Gleason’s 6 cancers are low grade, 7 is intermediate and 8 and above are high grade.
Risk Groups
A patient’s risk group is more important than Stage (NCCN) for most prostate cancer experts. Risk groups are determined by PSA, clinical stage and Gleason’s score. Groups range from very low to very high.
- Low risk – PSA < 10, Gleason’s 6, Clinical stage T2a or less.
- Intermediate risk – PSA 10-20, Gleason’s 7, T2b-2c.
- High risk – PSA >20, Gleason’s 8 and above, T3a or higher.
Your prostate cancer treatment options depend on your overall health and your risk group classification. There are only three acceptable options of treatment for localized prostate cancer: Active surveillance, surgery and radiation therapy.
- Active surveillance
- For men diagnosed with low-risk prostate cancer, treatment may not be necessary immediately and some men may never need treatment. In active surveillance, regular follow-up blood tests, rectal exams and possibly MRIs and biopsies may be performed to monitor for progression of your cancer. If tests show your cancer is progressing, you may opt for a prostate cancer treatment such as surgery or radiation.
- Surgery to remove the prostate
- Surgical treatment for prostate cancer involves removing the entire prostate, the seminal vesicles and sometimes also some lymph nodes in the pelvis. There are two types of prostatectomies: open and robotic-assisted. Most are robotic assisted currently. Radical prostatectomy carries a risk of urinary incontinence and erectile dysfunction.
- Radiation therapy or radiotherapy
- Radiation therapy uses high-powered energy to kill cancer cells. Prostate cancer radiation therapy can be delivered in two ways:
- Externally (External Beam Radiation Therapy – EBRT)
- During external beam radiation therapy, you lie on a table while a machine moves around your body, directing high-powered X-rays to your prostate cancer. You typically undergo external beam radiation treatments five days a week for typically 8-9 weeks or for 5 weeks if combined with brachytherapy. Modern day techniques include IMRT and VMAT.
- Alternatively, a technique called Stereotactic Body Radiation Therapy (SBRT) or Stereotactic Ablative Radiotherapy (SABR) can be used. This involves typically 5 days of treatment over two weeks time delivering much higher daily doses of radiation therapy. Many machine platforms have such capabilities including the Radixact.
- For EBRT, Texas Radiotherapy utilizes both IMRT and SBRT to treat prostate cancer.
- Proper targeting of the prostate is important since the prostate is shifted day-to-day by differences in fullness of the bladder and rectum. In order to account for the position changes, gold fiducial markers are placed into the prostate so that x-ray images can localize the markers and ensure accurate radiation therapy.
- Internally (Brachytherapy)
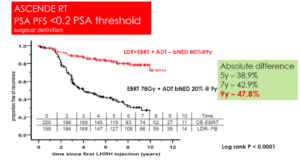
- Brachytherapy involves placing many rice-sized radioactive seeds in the prostate gland under ultrasound guidance. The radioactive seeds deliver high doses of radiation to a very confined region and thus the much higher doses of radiation therapy can be delivered than with any other technique. Since higher doses can be delivered with brachytherapy than with any other means, brachytherapy is the “gold standard” of radiation therapy for low- and favorable intermediate-risk patients (monotherapy = brachytherapy alone) or in combination therapy (brachytherapy plus external beam radiation therapy, EBRT) in unfavorable intermediate- or high-risk patients). A recent clinical trial (ASCENDE-RT) concluded that intermediate- or high-risk patients that received combination therapy were twice as likely to have PSA control of their cancers than patients who received EBRT alone. (https://doi.org/10.1016/j.ijrobp 2016.11.026)
- At Texas Radiotherapy, we perform the next generation of brachytherapy or prostate seed implants known as MRI-assisted radiosurgery (MARS). MRI imaging is utilized to design and guide the placement of the radioactive seeds during the implant procedure, which leads to better and safer seed implants than without MRI-assistance.
- Brachytherapy involves placing many rice-sized radioactive seeds in the prostate gland under ultrasound guidance. The radioactive seeds deliver high doses of radiation to a very confined region and thus the much higher doses of radiation therapy can be delivered than with any other technique. Since higher doses can be delivered with brachytherapy than with any other means, brachytherapy is the “gold standard” of radiation therapy for low- and favorable intermediate-risk patients (monotherapy = brachytherapy alone) or in combination therapy (brachytherapy plus external beam radiation therapy, EBRT) in unfavorable intermediate- or high-risk patients). A recent clinical trial (ASCENDE-RT) concluded that intermediate- or high-risk patients that received combination therapy were twice as likely to have PSA control of their cancers than patients who received EBRT alone. (https://doi.org/10.1016/j.ijrobp 2016.11.026)
Side effects of radiation therapy can include painful, frequent or urgent urination, as well as rectal symptoms such as loose stools or pain when passing stools. Erectile dysfunction can also occur.
- Hormone therapy
- Hormone therapy or androgen deprivation therapy (ADT) is often used in combination with radiation therapy. ADT is a treatment to stop your body from producing the male hormone testosterone, which the prostate cancer cells use as “food”. ADT is commonly given as injections that typically last anywhere from 1 – 6 months or in pill form. ADT temporarily puts the prostate cancer to sleep. It also will shrink the size of the prostate and it works in conjunction with radiation therapy to improve treatment results. Side effects include fatigue, mood changes, hot flashes, weight gain, loss of libido and inability to have erections.
Comparing Treatments
For an objective, easy to use and interactive comparison of treatment results for all treatments of localized prostate cancer by risk group, view The Prostate Cancer Results Study Group at www.prostatecancerfree.org. This is a comparison of all available studies published in the literature which are updated annually and organized by well-respected Radiation Oncologists and Urologists. The Disease-Free Survival (DFS) is analyzed by Risk Group (Low, Intermediate, and High). For each of the Risk Groups, the DFS for patients treated with Brachytherapy alone in low risk patients, or combined with External Radiation and/or Androgen Blockade for intermediate- and high-risk patients, is superior to any of the other treatments, including Radical Prostatectomy and External Radiation.
Side effects of radiation therapy for prostate cancer can include bowel problems such as loose stools and rectal fullness. This is due to the prostate and rectum being in close proximity to each other. Therefore, even with the most advanced forms of radiation treatment, a small sliver of the rectum can receive radiation therapy. Hydrogel spacers, such as Barrigel or SpaceOAR, can create space between the prostate and rectum, moving the rectum out of radiation beam exposure. Hydrogel spacers provide for safer radiation therapy and result in less complications.